Optimization of pharmacotherapeutic options in sarcoidosis
The clinical presentation and course of sarcoidosis are highly variable, varying from minimal involvement to derangement of organ physiology with functional impairment. Most sarcoidosis patients show spontaneous resolution, but in patients with a severe disease course and poor prognosis, a timely implementation of an appropriate potent individual pharmacological treatment regimen is important. Despite the availability of several immunosuppressive therapeutic options in sarcoidosis, there is a lack of standardized management strategies. The published data on the different pharmacological therapeutics are limited. The studies performed in this research project evaluate several aspects of therapeutic options in sarcoidosis with the aim of improving the management of patients who require pharmacological treatment.
This research project was started with the evaluation of the extent, distribution and consistency of organ involvement detected by fluorine18-fluorodeoxyglucose positron emission tomography/computed tomography (18F-FDG PET/CT or PET) in sarcoidosis patients with persistent disabling symptoms. Positive PET findings were classified as thoracic and/or extrathoracic. Involvement of individual organs was assessed as well.
The next project investigates the prevalence of muscle atrophy and cachexia in Dutch sarcoidosis patients, and the association of these body composition profiles with sarcoidosis disease activity and severity. Fat-free mass was assessed as an indirect measure of muscle mass by bioelectrical impedance analysis. Patients were stratified based on body mass index (BMI) and fat-free mass index (FFMI). The aim was to establish if muscle atrophy and cachexia are frequent problems in sarcoidosis which should be taken into account in disease management.
The third part of the research project consists of the optimization of management of hepatic sarcoidosis and handling of liver-test abnormalities. Patients with hepatic involvement are usually asymptomatic, but in a significant number disabling symptoms can be present. Furthermore, sometimes hepatic sarcoidosis can be a rapid progressive disease with the occurrence of complications, such as liver cirrhosis. Diagnosis is difficult, as studies are scarce, diagnostic criteria are lacking and guidelines with recommendations for diagnosis and follow-up of patients suspected of hepatic sarcoidosis are not available. The presence and severity of liver-test abnormalities in a large cohort of patients with confirmed sarcoidosis was established. Additionally, the association between severity of liver-test abnormalities and histopathological abnormalities in hepatic sarcoidosis was evaluated. Furthermore, an overview of the knowledge available in the literature about therapeutic options for sarcoidosis liver involvement was given. The available data were combined into recommendations for the optimal therapeutic approach in clinical practice.
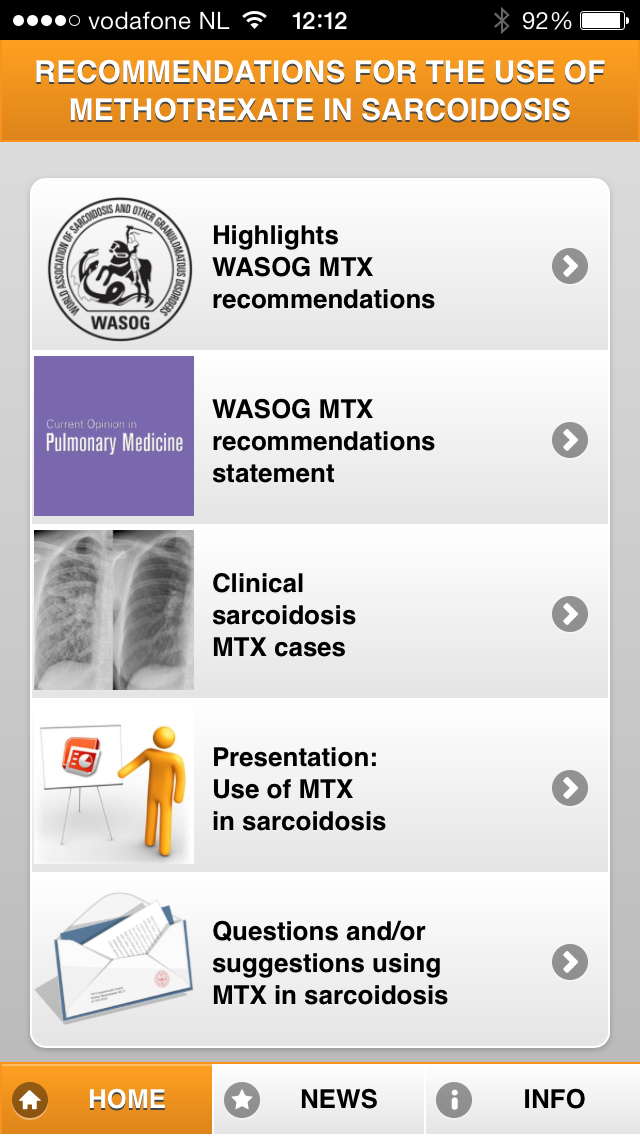
The development of practical recommendations, on behalf of the World Association of Sarcoidosis and Other Granulomatous Disorders (WASOG), for the use of methotrexate (MTX) in sarcoidosis by integrating the evidence obtained through a systematic literature review and the opinions of sarcoidosis experts worldwide, is presented in the next project. The recommendations, the complete statement, clinical cases and other information, are available in the app ‘MTX in sarcoidosis’. You can download it for free from the Apple Store or Google Play Store.
Practical recommendations are also developed for the use of the anti-TNF-α agents infliximab and adalimumab in sarcoidosis, by combining the evidence from both a systematic literature search and the expert opinions of the world’s leading sarcoidologists worldwide.
And finally, possible factors identifying responders to anti-TNF-α agents are explored. The association between the presence of the TNF-α G-308A polymorphism and the response to anti-TNF-α therapy amongst patients with refractory sarcoidosis was assessed.
This research project is supported by a research grant of the ild care foundation and Teva the Netherlands. Furthermore, this study is facilitated by Hospital Gelderse Vallei (ZGV), Ede, the Netherlands.
Researcher
Anne Cremers (1985) studied medicine at the Maastricht University, where she obtained her MD in 2010. In 2010 she started her training in internal medicine at the Atrium Medical Centre Heerlen, the Netherlands. In 2014 she will start her training in rheumatology at the Rijnstate Hospital in Arnhem and the University Medical Centre St Radboud Nijmegen, the Netherlands. In 2010 she started research activities in sarcoidosis at the Maastricht University Medical Centre+ (MUMC+), NL. At the 2010 meeting of the Dutch organization of Gastroenterology and Hepatology, and the WASOG/BAL conference in June 2011 in Maastricht, The Netherlands, she presented the study on liver-test abnormalities in sarcoidosis in an oral presentation and a poster, respectively. During the WASOG meeting in June 2013 in Paris, France, she presented the results of the study ‘Body composition profiling in sarcoidosis’ during a poster presentation. She also discussed the multinational survey and the development of recommendations for the use of methotrexate in sarcoidosis as an invited speaker at the 2013 AASOG meeting in Chicago, USA, and in a poster presentation during the 2013 WASOG meeting in Paris. June the 26th 2014 she finished her PhD thesis entitled: ‘Pharmacotherapeutic options in sarcoidosis: how can we improve them?’
Alles wat u altijd heeft willen weten over het gebruik van methotrexaat (MTX) bij sarcoïdose.
Dat kunt u vinden in een nieuwe handige app!
Met de ervaring van sarcoïdose experts en resultaten uit de literatuur worden 10 aanbevelingen gedaan hoe MTX te gebruiken in de praktijk. Het totale statement van de experts is ook beschikbaar. Tevens zijn er links naar de meest actuele studies op dit terrein. Klinische scenario’s die de behandeling met MTX duidelijk maken, zijn eveneens beschikbaar, evenals een paar klinische voorbeelden.
Deze app is een uitgave van de ild care foundation in samenwerking met de WASOG (www.wasog.org).
Informatie zal regelmatig worden geupdate. De app is helaas niet meer te downloaden.
Publications
- Cremers J, Drent M, Driessen A, Nieman F, Wijnen P, Baughman R, Koek G. Liver-test abnormalities in sarcoidosis. Eur J Gastroenterol Hepatol 2012; 24: 17-24.
- Cremers J, Drent M, Baughman R, Wijnen P, Koek G. Therapeutic approach of hepatic sarcoidosis. Curr Opin Pulm Med 2012; 18: 472-482.
- Cremers J, Drent M, Bast A, Shigemitsu H, Baughman R, Valeyre D, Sweiss N, Jansen T. Multinational evidence-based WASOG recommendations for the use of methotrexate in sarcoidosis: integrating systematic literature research and expert opinion of sarcoidologists worldwide. Curr Opin Pulm Med 2013; 19: 545-556. App ‘MTX in sarcoidosis’.
- Wijnen PA, Cremers JP, Nelemans PJ, Erckens RJ, Hoitsma E, Jansen TL, Bekers O, Drent M. Association of the TNF-α G-308A polymorphism with TNF-inhibitor response in refractory sarcoidosis. Eur Respir J 2014: Feb 20. [Epub ahead of print]
- Drent M, Cremers J, Jansen T. Sarcoidosis and the rheumatologist: therapeutic approach. Curr Opin Rheumatology 2014; 26(3): 276-284.
Name project: Optimization of pharmacotherapeutic options in sarcoidosis
Principal Investigator Drs. J.P. Cremers, Dept. of Internal Medicine, Atrium Heerlen, NL
Supervisors Prof. dr. M. Drent, head of ild care team, Hospital Gelderse Vallei Ede, Dept. of Toxicology, FHML, UM, Maastricht, NL and dr. T.L. Jansen, Department of Rheumatology, UMC St. Radboud Nijmegen, NL
Project team Prof. dr. M. Drent, dr. T.L. Jansen, dr. G.H. Koek, prof. dr. R.B. Baughman and dr. E.E. Lower, Cincinnati, USA, Dr. N, Sweiss, Chicago, USA
Period 2010-2014
Funded by A grant of the ild care foundation and Teva the Netherlands
Clinical trials NCT00626938
MEC number 04.145.11
Due to the retrospective character of this study and according to the criteria as mentioned above, approval by a Medical Ethics Committee was not required. Research with human subject’s falls under The Medical Research Involving Human Subjects Act (WMO) in the Netherlands. Studies involving human subjects must undergo a medical ethics review if they are subject to the Medical Research Involving Human Subjects Act (WMO).